05 Mar ODIN: Implementation of ODIN solutions on piloting sites
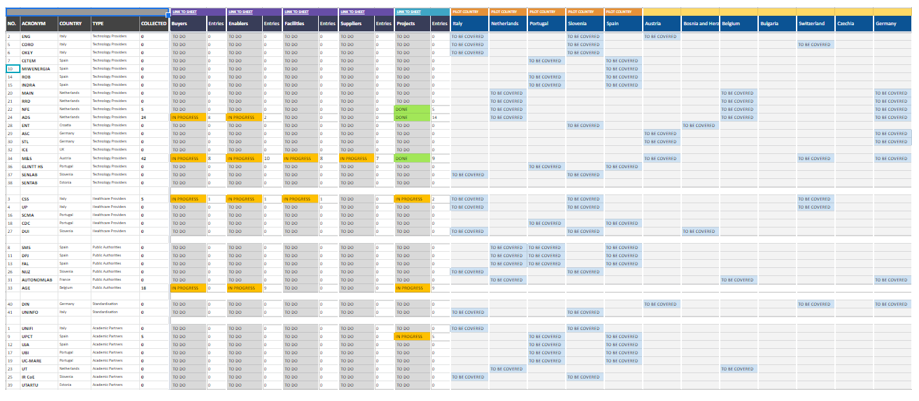
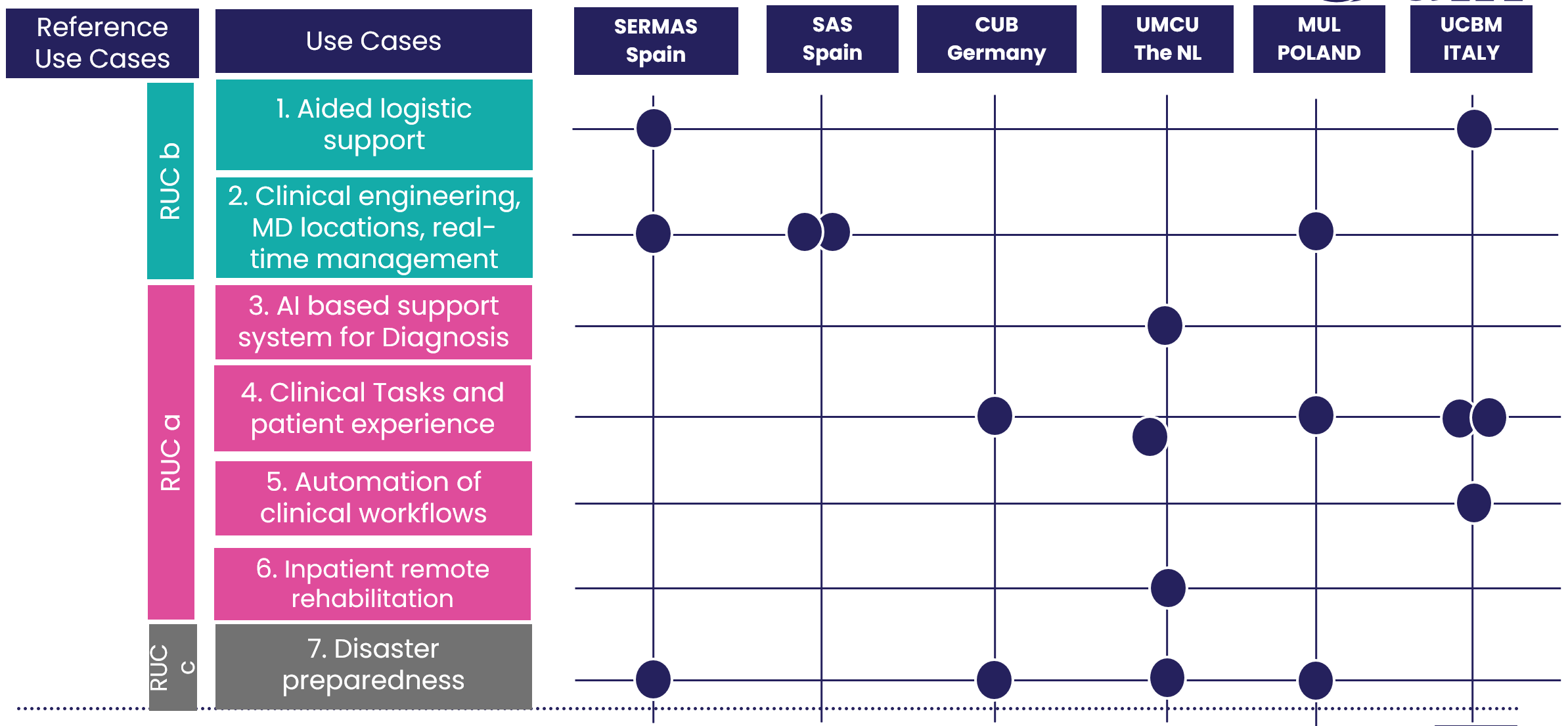
The ODIN piloting journey has begun: the piloting phase is conceptualised as a series of multicentre experiments, which aim to demonstrate the effectiveness and cost-effectiveness of Key Enabling Resources (KERs) such as Robots, AI, big-data and IoT, in EU hospitals.
When introducing new technologies or approaches into healthcare systems, it is essential to assess and demonstrate their impact on various stakeholders within the healthcare ecosystem, emphasizing both potential benefits and potential challenges. Impact assessment serves as a critical tool for planning and decision-making, enabling the analysis of effects of proposed projects.
To effectively conduct this analysis, it is essential to define a set of measurable Key Performance Indicators (KPIs) for impact assessment. These KPIs are tailored to specific project goals and outcomes expected from each Use Case (UC). They incorporate various scales and evaluation techniques, through a collaborative effort with the participating pilots. By establishing clear KPIs, this process ensures that the impact of new technologies can be accurately evaluated, supporting informed decision-making and confirming that the adopted technologies deliver meaningful improvements in hospital operations and patient care. Subsequently, in the context of evaluating the effectiveness of new technologies and approaches, Health Technology Assessment (HTA) has become increasingly important. It is a multidisciplinary process designed to assess new health technologies, encompassing diverse aspects such as medical, economic, organizational, social, and ethical considerations. Different types of analyses can be performed, depending on the KPIs and the outcomes of each use case.
Key take-aways from Impact Assessment
Cost-Effectiveness Varied by Use Case and Context. While cost-minimization analysis was applied to most use cases, only certain scenarios demonstrated clear financial savings. For instance, AI-assisted sleep disorder diagnosis at Charité and automated consumable delivery at SERMAS.
In contrast, cases where automation led to reduced manual workload but incurred high implementation costs, cost efficiency was not immediately achieved, as seen in MUL’s robotic blood sample transport and Real-Time Locating System (RTLS)-based equipment-tracking. These findings emphasize the need for scalability and broader deployment for financial viability.
Efficiency Gains and Workflow Optimization. Across all pilots, automation and digitalization consistently led to improved efficiency in hospital workflows by reducing manual tasks. For example, automated stent delivery at SERMAS and robot-assisted consumable transport at UMCU.
Real-time data transmission, such as RTLS for equipment-tracking at MUL and pathogen-monitoring at UMCU, demonstrated significant time savings for hospital staff, though financial viability depended on scale and system-wide integration.
AI-powered diagnostics, for instance Charité’s automated sleep scoring, showed great potential in reducing clinician workload, enhancing accuracy, and streamlining procedures.
Impact on Healthcare Personnel and Patient Experience. Robotic automation in logistics freed up nursing and clinical staff for more critical patient care tasks, leading to higher staff satisfaction in use cases where time-consuming duties were offloaded.
The introduction of smart patient monitoring and intervention systems, such as UCBM’s AI-assisted food intake monitoring, contributed to improved patient adherence to treatment and prevention measures.
Disaster preparedness applications, including UMCU’s simulated patients and MUL’s biohazard transport, reinforced the importance of technology-driven risk mitigation for future healthcare crises.
Scalability and Integration are Critical. The financial sustainability of many use cases is dependent on system-wide implementation, integration with existing hospital workflows, and scaling beyond pilot settings.
Links
https://odin-smarthospitals.eu/
https://odin-smarthospitals.eu/public-deliverables/
https://odin-smarthospitals.eu/wp-content/uploads/2023/05/Odin-Brochure-RUCS-A5-0.3.pdf
Keywords
Reference Use Cases, piloting, impact assessment, ODIN solutions, hospital management